Comparative Efficacy: Vaporized vs. Nebulized Cannabinoids for Pulmonary Delivery in Respiratory Conditions
Introduction
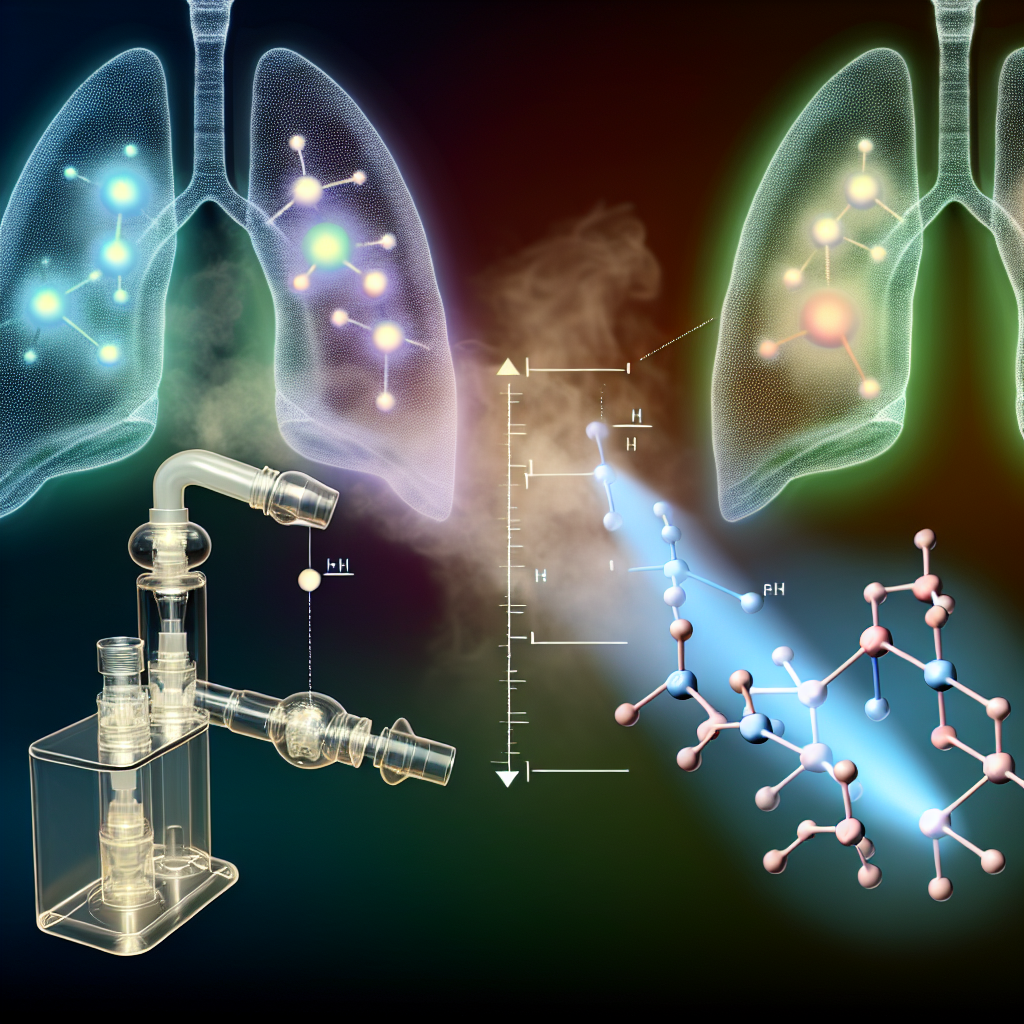
Cannabis-based therapies are reshaping treatment protocols for chronic diseases, particularly in pulmonary healthcare. Among the evolving therapeutic options, the use of cannabinoids for respiratory conditions such as asthma, chronic obstructive pulmonary disease (COPD), and pulmonary fibrosis is gaining momentum due to promising anti-inflammatory, immunomodulatory, and bronchodilatory effects.
Historically, smoking was the most common method for administering THC (tetrahydrocannabinol) and CBD (cannabidiol). Today, consumers and researchers alike seek safer and more precise pulmonary delivery methods—primarily vaporization and nebulization.
Vaporization involves heating cannabis (either flower or concentrates) to release cannabinoids without combustion, giving near-instantaneous relief. This method bypasses the gastrointestinal tract, avoids first-pass metabolism, and facilitates rapid absorption through alveolar tissue.
In contrast, nebulization transforms liquid cannabinoid formulations into fine aerosols, similar to how traditional inhalers for asthma and COPD deliver medications. This allows for controlled, deep lung distribution and reduces exposure to high-temperature byproducts.
Understanding which approach offers superior safety, bioavailability, and symptom control is critical for personalized therapeutics. This comparison informs product development, clinical practice, and patient use in an evolving landscape of inhaled cannabinoid treatment.
Vaporization: Mechanism, Benefits, and Drawbacks
Vaporization is well-established both clinically and recreationally. It delivers effects rapidly—typically within 1–5 minutes—through direct alveolar absorption. Devices vary from desktop vaporizers to handheld pen-style units, with some allowing temperature control to modulate cannabinoid and terpene activation.
According to a foundational study by Dr. Franjo Grotenhermen published in the Journal of Clinical Pharmacology, vaporized cannabinoids demonstrated a bioavailability range of 10–35%, often exceeding combustion methods due to reduced cannabinoid degradation.
However, one caveat arises under high-temperature settings. Per the MAPS-NORML vaporizer study, overheating cannabis can lead to the release of volatile organic compounds like benzene and toluene. While less toxic than cigarette smoke, these compounds may irritate airways over time, especially in patients with chronic inflammation.
Despite these concerns, the portability of vaporizers and near-instant relief they provide continue to make them a preferred method for acute symptom flares, anxiety, or pain modulation.
Nebulization: Precision Medicine and Therapeutic Evolution
Nebulized cannabinoid delivery is gaining traction through pharmaceutical innovation. It employs liquid formulations—like emulsified cannabinoids or water-soluble nanoparticles—delivered via medical-grade nebulizers or inhalers. Unlike vaporization, this process avoids combustion entirely, reducing respiratory burden.
The Israeli start-up Syqe Medical made headlines with a selective-dose THC inhaler. Their 2016 clinical trial published in the European Journal of Pain found that microdosed, aerosolized THC delivered effective pain relief with reduced psychoactive effects and minimal cognitive disruption. This precision dosing is especially valuable for long-term treatment protocols and for patients sensitive to THC’s psychoactivity.
In parallel, a pilot study by Sava Healthcare exploring ultrasonic nebulization of water-soluble CBD showed a 2–3x improvement in systemic bioavailability compared to vaping. This elevated absorption ensures more reliable therapeutic outcomes, ideal for conditions like chronic bronchitis or emphysema, where pulmonary function is compromised.
Aerosol particle size (1–5 microns) also plays a pivotal role, enabling deep lung penetration and optimizing interaction with CB1 and CB2 receptors—key modulators of inflammation, immune response, and bronchial tone. Additionally, absent thermal decomposition preserves cannabinoid integrity and safeguards against toxic inhalant formation.
However, challenges specific to nebulization include formulation stability, device cost, and the need for pharmaceutical-grade input materials. Addressing these issues is becoming more feasible as nanotechnology and drug delivery systems evolve.
Clinical Implications and Future Outlook
Taken together, current findings suggest that both vaporization and nebulization hold value, but in distinct clinical contexts. Vaporization is suited for on-demand relief and favorable for users seeking immediate effects, especially in acute respiratory distress. However, long-term risk due to residual thermal byproducts may limit its role in daily therapeutic use for vulnerable respiratory patients.
Nebulization emerges as a next-generation cannabis therapy, bringing higher precision, better tolerability, and superior pulmonary targeting. As device engineering and cannabinoid formulation science continue to advance, nebulization is likely to transform into a mainstay of respiratory cannabis medicine.
Expanded access to such technology through the regulated pharmaceutical pathway will not only enhance therapeutic outcomes but also contribute to a broader standardization of medical cannabis inhalation practices.
Conclusion
The comparison between vaporized and nebulized cannabinoid delivery marks a critical point in the evolution of inhaled cannabis therapies. For patients with compromised pulmonary health, nebulization is increasingly preferable thanks to its enhanced bioavailability, precision dosing, and absence of thermal byproducts. While vaporization remains effective and accessible, particularly for acute symptom control, it may not be optimal for long-term use in sensitive individuals. Ultimately, innovation in this space will drive safer, more personalized respiratory cannabinoid therapies backed by clinical rigor.
Concise Summary
Vaporization and nebulization represent two primary pulmonary cannabinoid delivery methods, each with unique advantages. Vaporization provides fast relief but may pose risks due to heat byproducts. In contrast, nebulization offers precise, deep lung delivery of cannabinoids—making it ideal for chronic respiratory conditions. Clinical studies show nebulized THC and CBD formulations offer greater bioavailability, reduced psychoactivity, and improved tolerability. As technology evolves, nebulization is poised to become the preferred method for therapeutic cannabinoid use in respiratory medicine, especially for asthma, COPD, and pulmonary fibrosis.
References
– Grotenhermen, F. (2003). Pharmacokinetics and pharmacodynamics of cannabinoids. Journal of Clinical Pharmacology
– MAPS-NORML Vaporizer Temperature Study
– Eisenberg, E., et al. (2016). Inhaled Δ9-THC for chronic pain relief. European Journal of Pain
– Sava Healthcare Nebulized CBD Pilot. Press Release
– Syqe Medical Clinical Inhaler Data. Syqe Medical