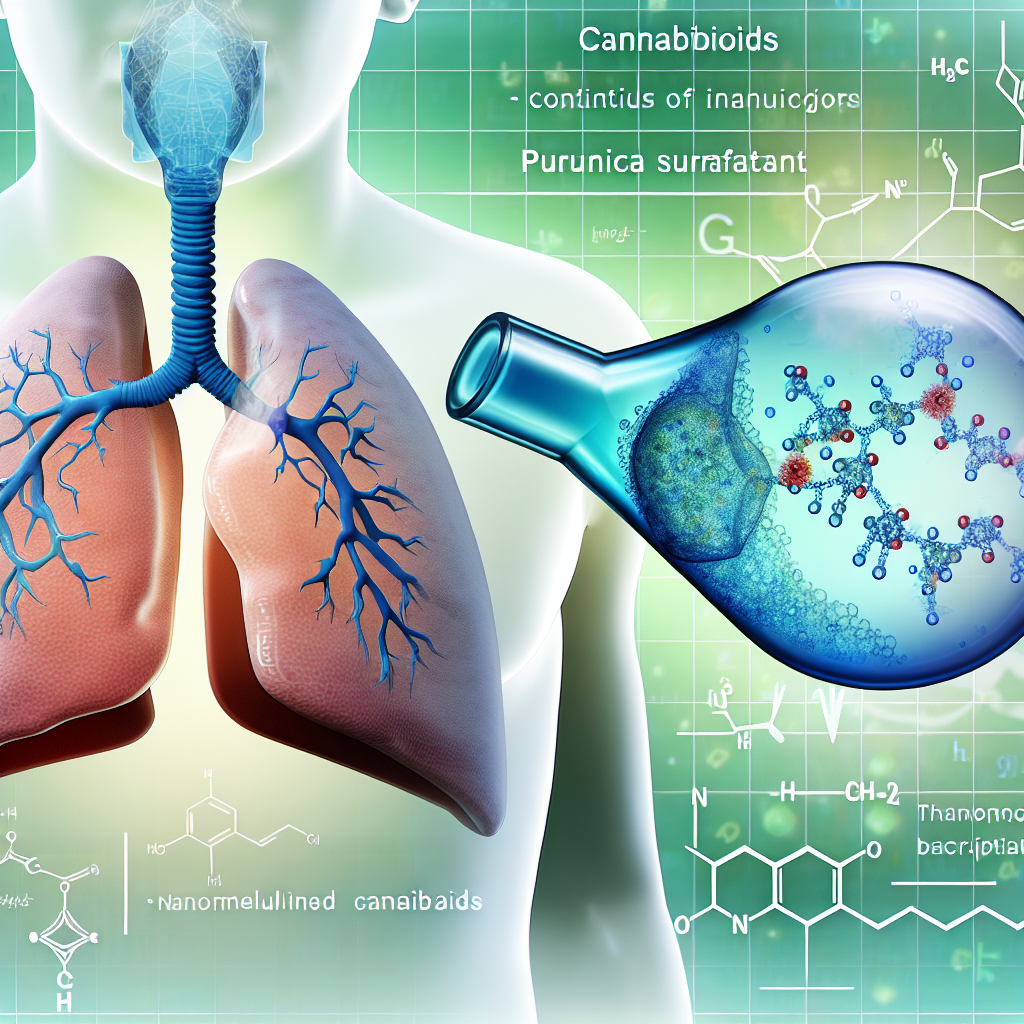
Pulmonary Surfactant-Based Nanoemulsions for Deep Lung Delivery of Cannabinoids
Introduction
Cannabis-based therapeutics are gaining traction in modern medicine as legalization spreads globally. However, optimizing the delivery of cannabinoids such as tetrahydrocannabinol (THC), cannabidiol (CBD), and cannabigerol (CBG) remains a challenge due to their poor bioavailability and inconsistent dosing profiles. Among administration routes, pulmonary delivery offers several advantages—fast onset, higher bioavailability than oral methods, and a non-invasive experience.
Traditional options like smoking and vaping suffer from limitations such as uneven dosing and possible lung irritation. In contrast, pulmonary surfactant-based nanoemulsions present an advanced method that leverages the lung’s natural mechanics. These nano-sized emulsions are designed to mimic the body’s lung surfactants—lipids and proteins that reduce surface tension in alveoli, thus facilitating smooth respiration and enhanced drug diffusion.
By incorporating cannabinoids into these nanoemulsions, it’s now possible to improve their water solubility and pharmacokinetics. Oral cannabinoids suffer from first-pass metabolism, dramatically reducing their efficacy. Inhaling cannabinoids through surfactant-assisted systems bypasses this issue and promotes controlled, accurate, and non-combustive administration.
Beyond general enhancements in efficacy, this approach allows for the customization of droplet size to target specific lung regions, such as bronchi or alveoli. This precision makes it appealing for treating conditions like chronic pain, neurological disorders, epilepsy, and even pulmonary inflammation.
As innovation in pulmonary drug delivery systems accelerates, the intersection of cannabis pharmacology and nanotechnology is fostering a new era of therapies that are safer, faster-acting, and more effective.
Features and Scientific Validation
The deep lung region—especially the alveolar sacs—offers an ideal site for systemic drug uptake thanks to its large surface area (around 70 square meters), its thin lining, and robust blood supply. Yet lipophilic compounds like THC and CBD struggle to reach this zone without assistance. Enter nanoemulsion technology enhanced by pulmonary surfactants.
These surfactants—comprising phospholipids such as dipalmitoylphosphatidylcholine (DPPC) and proteins like SP-A, SP-B, SP-C, and SP-D—naturally reduce alveolar surface tension, a feature leveraged in synthetic delivery systems to enhance absorption. Studies validate this delivery technology’s efficacy and safety.
A study in the journal Therapeutic Delivery demonstrated the use of DPPC-stabilized nanoemulsions to encapsulate lipophilic drugs, improving lung deposition and bioavailability without cytotoxicity. Additionally, these emulsions offer a sustained release profile, crucial for maintaining therapeutic cannabinoid levels over time.
Research in Advanced Drug Delivery Reviews reported that these systems can optimize aerosol droplet size (~100–200 nm), enabling deeper penetration into the lungs and reducing the risk of macrophage clearance, which often hinders the efficacy of inhaled medications.
A pivotal study published in Frontiers in Pharmacology in 2022 observed that CBD-loaded nanoemulsions formulated with natural pulmonary surfactants yielded significantly higher plasma concentrations in rodents than oral administration. This underpins the potential for accurately dosed, side-effect-reduced inhalable therapies, especially crucial during emergencies like seizure activity or acute pain.
From a manufacturing perspective, emulsification involves high-shear mixing or ultrasonic processing to create stable nanodroplets. These can encapsulate both hydrophilic and lipophilic compounds, enabling full-spectrum cannabinoid formulations—something that oral or smoked routes cannot reliably support.
This formulation flexibility is critical for therapeutic innovation. In particular, synergy among multiple cannabinoids (the so-called ‘entourage effect’) can be better realized through controlled inhalable methods. Coupled with customizable drug release and deeper lung targeting, this technology could transform routine cannabis-based therapies into advanced, precision-dose treatments.
Regulation is also catching up. Inhalable nanoemulsions must meet FDA or EMA safety and efficacy standards, including toxicological safety, surfactant biocompatibility, and natural lung function preservation. Encouragingly, biotech firms are reporting success in crossing early-stage regulatory thresholds by leveraging biocompatible materials and reproducible particle design.
Conclusion
Pulmonary surfactant-based nanoemulsions are poised to revolutionize cannabinoid delivery by overcoming traditional barriers to lung absorption and maximizing systemic availability. Offering precision dosing, improved bioavailability, and targeted site delivery, this cutting-edge approach merges nanotechnology with natural lung function. As legal and medical cannabis markets evolve, understanding and adopting this inhalable innovation will be key for industry professionals seeking to offer safer, faster, and more reliable treatments using globally recognized cannabinoid therapies.
Concise Summary
Pulmonary surfactant-based nanoemulsions offer a powerful solution for delivering cannabinoids like THC and CBD directly to deep lung tissue, improving bioavailability and reducing health risks compared to smoking or oral ingestion. Mimicking the lung’s natural surfactant system, this technology enables precise dosing, rapid onset, and sustained release. Backed by recent clinical studies, these inhalable nanoemulsions promise to transform cannabinoid therapy for conditions such as chronic pain, epilepsy, and anxiety. With increasing regulatory clarity, this innovation aligns biomedical engineering with cannabinoid medicine, setting a new standard in safe, effective cannabis-based therapeutics.
References
– Frontiers in Pharmacology, “Cannabidiol-loaded nanoemulsions for deep lung delivery”
– Therapeutic Delivery, “Lung-targeted nanoemulsions for respiratory drug administration”