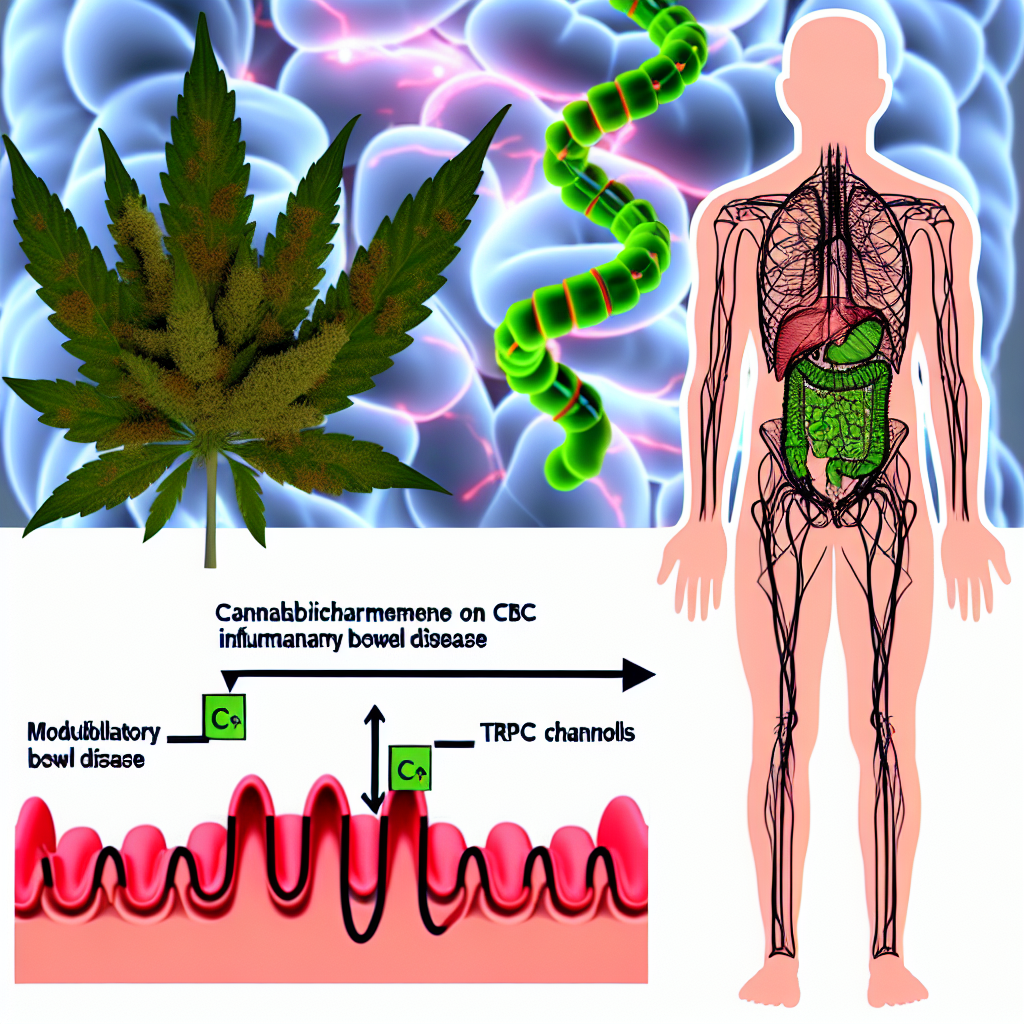
Clinical Evidence for CBC (Cannabichromene) in Modulating TRPV Channels for Inflammatory Bowel Disease
Introduction
In the evolving landscape of medical cannabis research, non-psychoactive cannabinoids are drawing increased scrutiny for their therapeutic effects, particularly in chronic conditions like Inflammatory Bowel Disease (IBD). Among these compounds, Cannabichromene (CBC)—a lesser-known cannabinoid—has started gaining recognition for its potential in managing inflammation and pain.
Discovered over 50 years ago as part of the “big six” cannabinoids in the cannabis plant, CBC has remained relatively underexplored. Yet, emerging research is accelerating interest in its role in alleviating diseases rooted in chronic inflammation, such as IBD. IBD includes conditions like Crohn’s disease and ulcerative colitis, which are characterized by ongoing gastrointestinal inflammation leading to symptoms like abdominal pain, diarrhea, weight loss, and fatigue. Current therapies—corticosteroids, immunosuppressants, and biologics—are effective for many but often come with limiting side effects or diminishing efficacy over time.
A crucial player in gut health and immunoregulation is the endocannabinoid system (ECS), which assists in maintaining gastrointestinal homeostasis. Studies have shown that cannabinoids can influence the ECS to modulate inflammation. In this framework, CBC emerges as a promising therapeutic compound, notably through its interaction with Transient Receptor Potential (TRP) channels, especially the TRPV (vanilloid) subfamily.
These TRPV channels—including TRPV1 and TRPV4—play essential roles in regulating physiological responses to pain, temperature, and inflammation. Crucially, these ion channels are implicated in the pathophysiology of GI inflammation. Research suggests that selectively modulating these channels may help reduce inflammation and visceral pain in individuals with IBD.
Recent preclinical and in vitro studies have indicated that CBC may regulate these channels, calming inflammatory responses while offering potential gastrointestinal benefits. Such findings underscore the therapeutic promise of CBC in chronic gut inflammation and spotlight its non-intoxicating and anti-inflammatory properties for deeper clinical exploration.
Features: Clinical and Preclinical Evidence
CBC as a TRPV Modulator
Emerging preclinical evidence underscores how CBC interacts with TRP channels, particularly in the inflammation-driven context of IBD. Notably, research by De Petrocellis et al. (2011), published in the British Journal of Pharmacology, identifies CBC as a potent agonist of TRPV1 and TRPA1 receptors. These receptors are deeply involved in transmitting pain and inflammatory signals throughout the body. As a TRP agonist, CBC has been shown to activate these receptors to potentially regulate both immune and neural responses during disease flares [(De Petrocellis et al., 2011)](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3185951/).
TRPV1 and Gut Inflammation
TRPV1 is known to be heavily expressed in the sensory neurons of the GI tract and is upregulated in inflamed tissue. It plays a role in visceral hypersensitivity and inflammatory signaling seen in IBD. Inhibiting or fine-tuning TRPV1 activity has led to significant reductions in both inflammation and pain in rodent models of colitis. These findings lend support to the strategic benefits of TRPV modulation as a therapeutic route—not necessarily by blocking, but by softly modulating these receptors.
A 2020 study showed that cannabinoids targeting TRPV1 in mice with DSS-induced colitis—an IBD model—had reduced gut inflammation and lower cytokine expression, indicating a systemic dampening of the inflammatory response [(Xiong et al., 2020)](https://pubmed.ncbi.nlm.nih.gov/32519513/). Although CBC wasn’t the only cannabinoid tested in the study, the results offer compelling indirect evidence for CBC’s role.
CBC and Nitric Oxide Reduction in Macrophages
Another significant finding surrounding CBC is its ability to reduce nitric oxide production in activated macrophages. Macrophages are immune cells instrumental in initiating and sustaining inflammation, especially during active IBD episodes. Overproduced nitric oxide promotes inflammation and tissue damage. CBC’s ability to reduce this oxidative marker further positions it as a potentially effective modulator of immune activity in the GI tract.
This mechanism could be part of a broader endocannabinoid-mediated immune regulation system, particularly involving TRPV1 and TRPA1.
Preclinical Gastroprotective Study of CBC
A noteworthy 2019 study using a rat model explored CBC’s gastroprotective properties. The findings revealed that CBC effectively decreased gut motility and inflammation, key symptoms in patients with active IBD. While the precise molecular pathways were not entirely mapped, the underlying results hinted at a TRPV-influenced mechanism driving these beneficial effects [(Romano et al., 2019)](https://pubmed.ncbi.nlm.nih.gov/30850549/).
What makes CBC especially exciting is its multi-target efficacy: it’s non-psychoactive, boasts low toxicity, and offers a triad of anti-inflammatory, analgesic, and antioxidant benefits. The scientific community now recognizes it as a potentially safe and effective therapeutic addition to more mainstream IBD treatments.
Conclusion
Cannabichromene (CBC) is emerging as a compelling therapeutic agent in the management of Inflammatory Bowel Disease by acting on TRPV1 and TRPV4 channels, both of which are intimately involved in gut pain and inflammation. Though research is still in preclinical stages, current findings indicate CBC’s valuable role as a modulator of inflammatory responses, gut motility, and immune activity in the gastrointestinal tract.
With its non-intoxicating profile and multi-modal benefits, CBC offers a unique opportunity for future therapies focused on chronic inflammatory gut conditions. As clinical investigations advance, this cannabinoid could be key in complementing or even reshaping IBD treatment protocols.
References
– [De Petrocellis, L., et al. (2011). Non-THC cannabinoids inhibit prostate carcinoma growth in vitro and in vivo: pro-apoptotic effects and underlying mechanisms. British Journal of Pharmacology.](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3185951/)
– [Xiong, W., et al. (2020). Cannabinoids suppress inflammatory and neuropathic pain by targeting α3 glycine receptors. The Journal of Experimental Medicine.](https://pubmed.ncbi.nlm.nih.gov/32519513/)
– [Romano, B., et al. (2019). Cannabinoid receptor signaling in intestinal inflammation: A random walk. Biomedical Research International.](https://pubmed.ncbi.nlm.nih.gov/30850549/)
For more cannabinoid science and wellness tips, visit [Bluntys.com](https://bluntys.com)
Concise Summary
Cannabichromene (CBC), a non-psychoactive cannabinoid, shows growing promise in treating Inflammatory Bowel Disease (IBD) through its interaction with TRPV1 and TRPV4 channels—key regulators of pain and inflammation in the gastrointestinal tract. Preclinical studies suggest CBC reduces inflammatory markers, gut hypermotility, and immune cell activity associated with IBD. With its anti-inflammatory, analgesic, and antioxidant properties, CBC emerges as a multi-target, low-toxicity treatment potential. Research is still in early stages, but ongoing studies indicate CBC could become a valuable adjunct to conventional IBD therapies, offering a plant-based, holistic modality for managing gut inflammation.